Rn 3.0 clinical judgment practice 1 – RN 3.0 Clinical Judgment Practice, an innovative approach to healthcare, revolutionizes the way nurses make clinical decisions. This comprehensive practice empowers nurses with the knowledge and skills to deliver optimal patient care, improve outcomes, and enhance the healthcare experience.
RN 3.0 Clinical Judgment Practice encompasses key components such as evidence-based practice, interprofessional collaboration, and patient-centered care. It provides a structured framework for nurses to navigate complex clinical scenarios, ensuring that decisions are informed, ethical, and aligned with the latest evidence.
RN 3.0 Clinical Judgment Practice
RN 3.0 Clinical Judgment Practice is a transformative approach to nursing care that empowers nurses to make critical decisions and provide optimal patient outcomes. It focuses on developing nurses’ clinical reasoning skills, enabling them to navigate complex healthcare situations and deliver evidence-based interventions.
RN 3.0 Clinical Judgment Practice is based on the American Nurses Association’s (ANA) Nurse Practice Model and incorporates the latest research and best practices in nursing care. It emphasizes the importance of critical thinking, clinical reasoning, and evidence-based practice.
Key Components of RN 3.0 Clinical Judgment Practice, Rn 3.0 clinical judgment practice 1
RN 3.0 Clinical Judgment Practice comprises several key components, including:
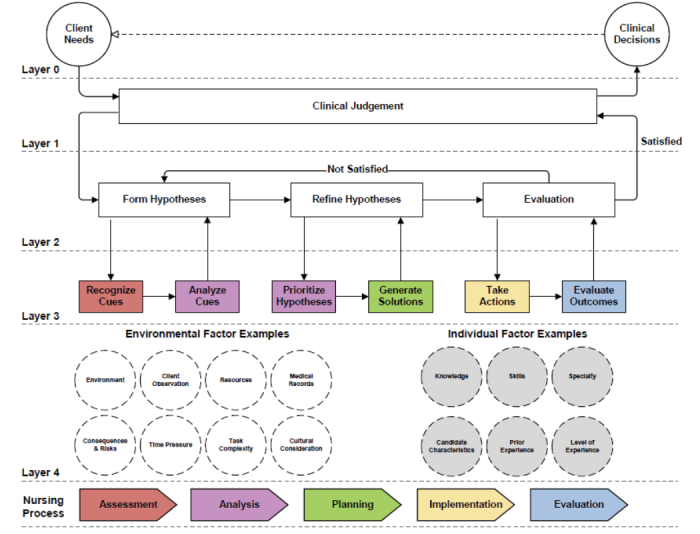
- Assessment: Gathering and interpreting patient data to identify problems and potential risks.
- Diagnosis: Identifying the patient’s health problems based on assessment findings.
- Planning: Developing a plan of care that Artikels interventions to address the patient’s problems.
- Implementation: Carrying out the plan of care and monitoring the patient’s response.
- Evaluation: Assessing the effectiveness of the plan of care and making necessary adjustments.
Clinical Decision-Making
Clinical judgment plays a crucial role in the effective decision-making process for nurses. It involves the integration of knowledge, experience, and critical thinking to assess patient situations, identify problems, and develop appropriate interventions.
The RN 3.0 Clinical Judgment Practice Artikels the following steps involved in clinical decision-making:
- Assessment:Gather data about the patient’s condition, including vital signs, medical history, and physical examination findings.
- Diagnosis:Analyze the data to identify the patient’s problem or condition.
- Planning:Develop a plan of care that includes interventions to address the patient’s needs.
- Implementation:Carry out the interventions and monitor the patient’s response.
- Evaluation:Assess the effectiveness of the interventions and make adjustments as necessary.
Strategies for Enhancing Clinical Decision-Making Skills
To enhance clinical decision-making skills, nurses can employ the following strategies:
- Critical Thinking:Develop critical thinking skills through education, practice, and self-reflection.
- Knowledge Acquisition:Continuously update knowledge and skills through ongoing education and research.
- Clinical Experience:Gain experience in diverse clinical settings to broaden exposure to various patient conditions.
- Collaboration:Consult with colleagues, physicians, and other healthcare professionals to gather multiple perspectives and expertise.
- Use of Evidence-Based Practice:Utilize research and evidence-based guidelines to support clinical decisions.
Evidence-Based Practice
Evidence-based practice (EBP) is a systematic approach to clinical decision-making that uses the best available evidence to guide practice. It is an essential component of RN 3.0 Clinical Judgment Practice, as it helps nurses to make decisions that are based on the latest research and best practices.
The principles of EBP include:
- Using the best available evidence to make decisions about patient care.
- Integrating evidence with clinical expertise and patient preferences.
- Evaluating the effectiveness of interventions and making changes as needed.
EBP has been shown to improve patient outcomes in a variety of settings. For example, a study published in the journal JAMA Internal Medicine found that patients who received care from nurses who used EBP had a lower risk of death, hospital readmission, and other adverse events.
Here are some examples of how EBP has improved patient outcomes:
- In the intensive care unit, EBP has been used to reduce the risk of ventilator-associated pneumonia.
- In the emergency department, EBP has been used to improve the triage process and reduce wait times.
- In the community setting, EBP has been used to improve the management of chronic diseases such as diabetes and heart failure.
EBP is an essential component of RN 3.0 Clinical Judgment Practice. It helps nurses to make decisions that are based on the best available evidence and improve patient outcomes.
Interprofessional Collaboration: Rn 3.0 Clinical Judgment Practice 1
Interprofessional collaboration is an essential aspect of RN 3.0 Clinical Judgment Practice, promoting improved patient outcomes and enhanced healthcare delivery. It involves healthcare professionals from various disciplines working together to provide comprehensive and coordinated care to patients. This collaborative approach enables the sharing of knowledge, skills, and perspectives, leading to better decision-making and patient-centered care.
Benefits of Interprofessional Collaboration
- Improved patient outcomes: By combining the expertise of different healthcare professionals, interprofessional collaboration ensures a comprehensive approach to patient care, leading to better health outcomes.
- Enhanced communication: Interprofessional collaboration fosters open communication and information sharing among healthcare professionals, reducing errors and improving patient safety.
- Increased efficiency: By coordinating care and avoiding duplication of efforts, interprofessional collaboration improves efficiency and optimizes resource utilization.
- Improved job satisfaction: Collaboration creates a positive and supportive work environment, enhancing job satisfaction and reducing burnout among healthcare professionals.
Challenges of Interprofessional Collaboration
- Communication barriers: Differences in professional language, jargon, and communication styles can create barriers to effective interprofessional collaboration.
- Role ambiguity: Unclear roles and responsibilities can lead to confusion and hinder collaboration.
- Power dynamics: Hierarchical structures and power imbalances can affect collaboration, with some professions having more influence than others.
- Time constraints: The busy nature of healthcare can make it challenging to find time for interprofessional collaboration.
Strategies for Fostering Effective Interprofessional Collaboration
- Establish clear roles and responsibilities: Defining the roles and responsibilities of each healthcare professional involved in patient care is crucial for effective collaboration.
- Promote open communication: Creating a culture of open communication and active listening among healthcare professionals is essential for effective collaboration.
- Encourage shared decision-making: Involving patients and their families in decision-making promotes patient-centered care and fosters collaboration among healthcare professionals.
- Provide education and training: Offering educational opportunities and training programs can enhance interprofessional communication, collaboration skills, and cultural sensitivity.
- Foster a positive work environment: Creating a positive and supportive work environment promotes collaboration and reduces barriers to teamwork.
Patient-Centered Care
Patient-centered care (PCC) is a healthcare approach that prioritizes the patient’s needs, values, and preferences. It recognizes that patients are unique individuals with their own experiences, beliefs, and expectations, and that their involvement in their own care is essential for achieving optimal outcomes.
PCC is integrated into RN 3.0 Clinical Judgment Practice through several key principles:
- Respect for patient autonomy:Nurses respect the patient’s right to make decisions about their own care, even if those decisions differ from the nurse’s own recommendations.
- Shared decision-making:Nurses work with patients to develop a shared understanding of the patient’s condition and treatment options, and to make decisions about care that are in line with the patient’s goals and values.
- Patient education:Nurses provide patients with the information they need to make informed decisions about their care, and to participate actively in their own care.
- Emotional support:Nurses provide emotional support to patients and their families, and help them to cope with the challenges of illness and treatment.
Importance of Patient Involvement in Decision-Making and Care Planning
Patient involvement in decision-making and care planning is essential for several reasons:
- Improved patient satisfaction:Patients who are involved in their own care are more likely to be satisfied with their care.
- Improved patient outcomes:Patients who are involved in their own care are more likely to adhere to treatment plans and to achieve better health outcomes.
- Reduced healthcare costs:Patient involvement in care planning can help to reduce healthcare costs by reducing the need for unnecessary tests and procedures.
Examples of How Patient-Centered Care Has Improved Patient Satisfaction and Outcomes
There are many examples of how patient-centered care has improved patient satisfaction and outcomes. For example, a study published in the journal JAMA Internal Medicine found that patients who received patient-centered care were more likely to report being satisfied with their care, and were more likely to adhere to their treatment plans.
Another study, published in the journal The Lancet, found that patients who received patient-centered care were more likely to achieve better health outcomes, such as lower blood pressure and improved cholesterol levels.
Ethical Considerations
In RN 3.0 Clinical Judgment Practice, ethical considerations are paramount, guiding nurses’ decision-making and actions to ensure the well-being and autonomy of patients.
The principles of ethical decision-making in healthcare, such as beneficence, non-maleficence, autonomy, and justice, serve as the foundation for ethical practice. Nurses must carefully weigh these principles when making decisions that impact patient care.
Navigating Ethical Dilemmas
Clinical practice often presents nurses with ethical dilemmas, where multiple ethical principles may conflict. To navigate these dilemmas effectively, nurses should:
- Identify the ethical issues involved.
- Gather relevant information and perspectives.
- Consider the potential benefits and harms of different courses of action.
- Seek guidance from colleagues, supervisors, or ethics committees when necessary.
- Make decisions that align with the patient’s values and preferences, while also considering the ethical principles of the profession.
FAQ Insights
What is the significance of RN 3.0 Clinical Judgment Practice?
RN 3.0 Clinical Judgment Practice enhances the quality and safety of patient care by promoting evidence-based decision-making, fostering interprofessional collaboration, and prioritizing patient-centered care.
How does RN 3.0 Clinical Judgment Practice differ from traditional nursing practice?
RN 3.0 Clinical Judgment Practice incorporates a more structured and systematic approach to clinical decision-making, emphasizing the use of evidence-based research and interprofessional collaboration to deliver optimal patient care.
What are the key components of RN 3.0 Clinical Judgment Practice?
RN 3.0 Clinical Judgment Practice consists of evidence-based practice, interprofessional collaboration, patient-centered care, ethical considerations, and clinical decision-making.