Components of blood worksheet answers – Embark on an illuminating journey into the intricate world of blood composition with our comprehensive worksheet answers. This meticulously crafted guide unveils the essential components of blood, their functions, and their significance in maintaining overall health.
Our in-depth exploration delves into the structure and roles of red blood cells, white blood cells, platelets, and plasma. We unravel the fascinating processes of blood clotting and blood transfusions, shedding light on their crucial implications in medicine and healthcare.
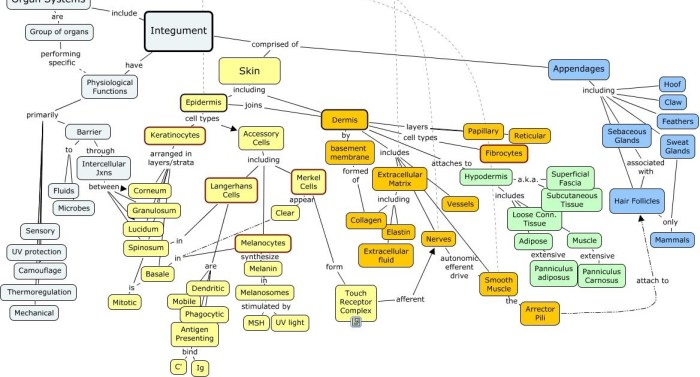
Blood Composition Overview
Blood is a complex fluid that circulates throughout the body, performing various vital functions. It consists of several major components, each with distinct roles in maintaining homeostasis and supporting physiological processes.
The primary components of blood include:
- Red blood cells (erythrocytes)
- White blood cells (leukocytes)
- Platelets (thrombocytes)
- Plasma
Functions of Blood Components
Red blood cellscontain hemoglobin, which binds to oxygen and transports it throughout the body. They are essential for cellular respiration and oxygen delivery to tissues.
White blood cellsare part of the immune system and defend the body against infections and foreign substances. They include various types, such as neutrophils, lymphocytes, and macrophages.
Plateletsplay a crucial role in blood clotting by aggregating and forming a plug to stop bleeding.
Plasmais the liquid component of blood that contains water, electrolytes, proteins, hormones, and nutrients. It maintains fluid balance, transports substances, and regulates osmotic pressure.
| Component | Function |
|---|---|
| Red blood cells | Oxygen transport |
| White blood cells | Immune defense |
| Platelets | Blood clotting |
| Plasma | Fluid balance, substance transport, osmotic regulation |
Red Blood Cells (Erythrocytes)
Red blood cells, also known as erythrocytes, are the most abundant type of blood cell. They are responsible for transporting oxygen from the lungs to the rest of the body.
Structure and Function of Red Blood Cells
Red blood cells are unique in that they lack a nucleus and most organelles. This allows them to be filled with hemoglobin, a protein that binds to oxygen. The lack of a nucleus also makes red blood cells flexible, allowing them to squeeze through narrow blood vessels.
Role of Hemoglobin in Oxygen Transport
Hemoglobin is a complex protein that contains iron. Each hemoglobin molecule can bind to four oxygen molecules. When red blood cells reach the lungs, hemoglobin binds to oxygen in the alveoli. The oxygenated red blood cells then travel through the bloodstream to the rest of the body, where they release the oxygen to cells.
Production and Lifespan of Red Blood Cells
Red blood cells are produced in the bone marrow. The lifespan of a red blood cell is about 120 days. After this time, the red blood cells are broken down in the spleen and liver.
White Blood Cells (Leukocytes)
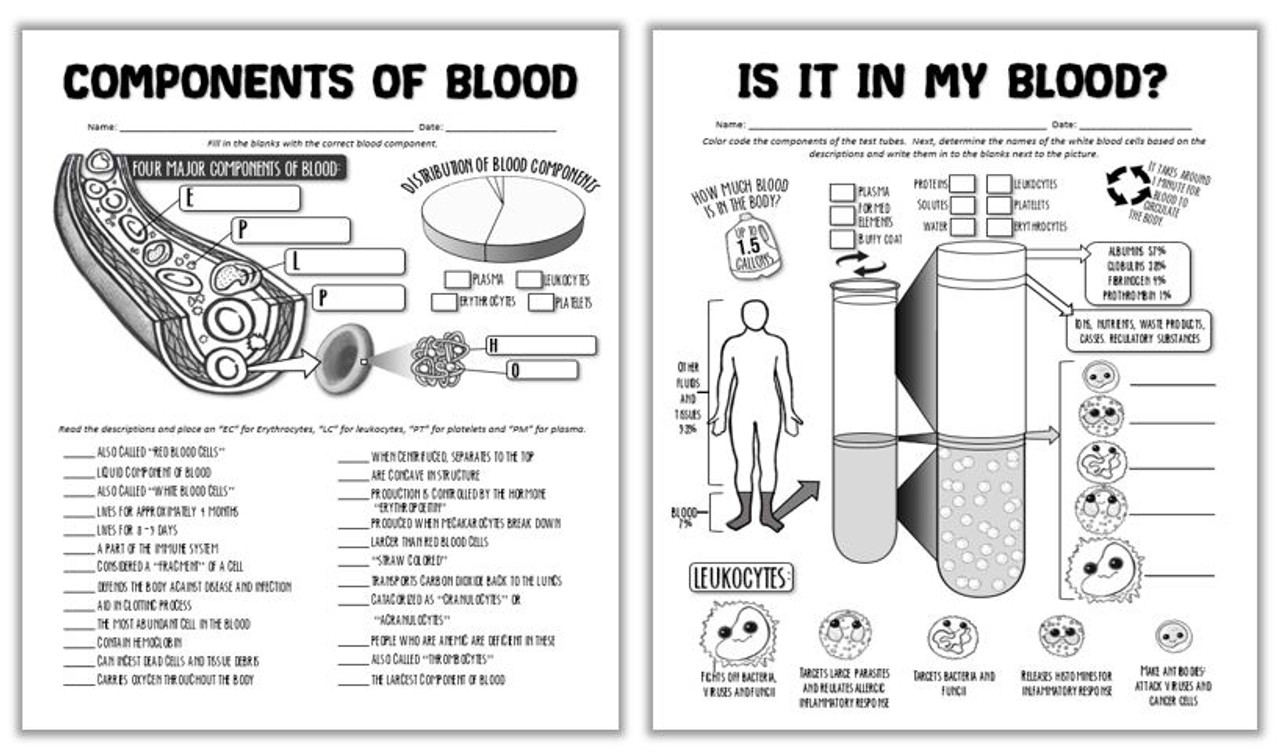
White blood cells (leukocytes) are an essential component of the body’s immune system, responsible for protecting the body from infections and foreign substances.
There are several types of white blood cells, each with a specific role in the immune response:
Types of White Blood Cells
- Neutrophils:The most common type of white blood cell, neutrophils are phagocytic cells that engulf and destroy bacteria and other microorganisms.
- Eosinophils:Eosinophils are involved in the body’s response to allergic reactions and parasitic infections.
- Basophils:Basophils are involved in the release of histamine and other inflammatory mediators.
- Lymphocytes:Lymphocytes are responsible for the body’s adaptive immune response, which involves the production of antibodies and the activation of other immune cells.
- Monocytes:Monocytes are phagocytic cells that differentiate into macrophages, which are involved in the removal of cellular debris and the presentation of antigens to the immune system.
Role of White Blood Cells in the Immune System, Components of blood worksheet answers
White blood cells play a crucial role in the immune system by:
- Recognizing and destroying pathogens, such as bacteria, viruses, and parasites.
- Producing antibodies to neutralize pathogens.
- Activating other immune cells, such as macrophages and natural killer cells.
- Regulating the immune response to prevent excessive inflammation.
Production and Lifespan of White Blood Cells
White blood cells are produced in the bone marrow and circulate in the bloodstream for several hours to days. The lifespan of white blood cells varies depending on the type of cell, with neutrophils having a lifespan of only a few days, while lymphocytes can live for months or even years.
Platelets (Thrombocytes)
Platelets, also known as thrombocytes, are small, disk-shaped blood cells that play a vital role in hemostasis, the process of stopping bleeding.
Structure of Platelets
Platelets are produced from the fragmentation of large cells called megakaryocytes in the bone marrow. They are about 2-3 micrometers in diameter and have a unique structure that enables them to perform their functions.
- Central Granules:Contain proteins essential for blood clotting, such as fibrinogen, von Willebrand factor, and platelet factor 4.
- Dense Granules:Store adenosine diphosphate (ADP), serotonin, and calcium ions, which are released during platelet activation.
- Mitochondria:Provide energy for platelet function.
- Glycocalyx:A layer of carbohydrates on the platelet surface that helps them interact with other blood cells and the blood vessel wall.
- Plasma Membrane:Contains receptors for various clotting factors and adhesive proteins.
Function of Platelets
The primary function of platelets is to prevent and stop bleeding by forming a clot at the site of a damaged blood vessel. This process involves three main steps:
- Adhesion:Platelets adhere to the damaged blood vessel wall at the site of injury, forming a temporary plug.
- Aggregation:Additional platelets are recruited to the site and aggregate together, forming a stable clot.
- Clot Retraction:The clot contracts, reducing its size and strengthening the seal.
Plasma
Plasma, the liquid component of blood, constitutes approximately 55% of its volume. It is a complex mixture of water, electrolytes, proteins, hormones, waste products, and gases.
The primary function of plasma is to maintain blood volume and transport substances throughout the body. It provides a medium for the exchange of nutrients, hormones, and waste products between the blood and tissues.
Plasma Proteins
Plasma proteins, which account for about 7% of plasma volume, play crucial roles in maintaining blood volume and transporting substances.
- Albumin:The most abundant plasma protein, albumin contributes significantly to osmotic pressure, which helps maintain blood volume.
- Globulins:These proteins include immunoglobulins (antibodies) that provide immunity, as well as transport proteins that carry hormones, lipids, and vitamins.
- Fibrinogen:This protein is essential for blood clotting.
Production and Lifespan of Plasma
Plasma is produced in the liver and has a lifespan of about 10-12 days. During this time, it circulates throughout the body, performing its various functions. Plasma proteins are continuously synthesized and degraded to maintain their concentration within a narrow range.
Blood Clotting
Blood clotting, also known as hemostasis, is a complex physiological process that helps prevent excessive bleeding and maintains the integrity of the circulatory system. When blood vessels are damaged, a series of biochemical reactions occur to form a blood clot that seals the breach and prevents further blood loss.
The process of blood clotting involves the activation of platelets and the coagulation cascade, a series of enzymatic reactions that ultimately lead to the formation of a fibrin clot.
Factors Involved in Blood Clotting
Several factors are involved in blood clotting, including:
- Platelets:Platelets are small, disk-shaped cells that are activated when blood vessels are damaged. They aggregate at the site of injury and release factors that initiate the coagulation cascade.
- Coagulation factors:Coagulation factors are proteins that circulate in the blood and are activated in a sequential manner to form a fibrin clot. The most important coagulation factor is fibrinogen, which is converted to fibrin by the enzyme thrombin.
- Vitamin K:Vitamin K is an essential nutrient that is required for the synthesis of several coagulation factors.
Importance of Blood Clotting
Blood clotting is essential for preventing excessive bleeding and maintaining the integrity of the circulatory system. Without blood clotting, even minor injuries could lead to life-threatening hemorrhage. The blood clot forms a temporary seal over the damaged blood vessel, allowing the underlying tissues to heal.
However, excessive blood clotting can also be a problem, as it can lead to the formation of blood clots in the arteries or veins, which can block blood flow and cause serious health problems, such as heart attack or stroke.
Blood Transfusions: Components Of Blood Worksheet Answers
Blood transfusions involve the transfer of blood or blood components from one individual (the donor) to another (the recipient) to address various medical conditions. Understanding blood types and their compatibility is crucial for safe and effective transfusions.
Blood Types and Compatibility
Blood types are determined by the presence or absence of specific antigens, which are proteins found on the surface of red blood cells. The ABO blood group system and the Rh factor are the most significant blood typing systems.
- ABO Blood Group System:Individuals have one of four blood types: A, B, AB, or O. Type A blood has A antigens, type B has B antigens, type AB has both A and B antigens, and type O has neither.
- Rh Factor:The Rh factor is another antigen. Individuals who have the Rh factor are Rh-positive (Rh+), while those who lack it are Rh-negative (Rh-).
Blood transfusions must be compatible with the recipient’s blood type to prevent immune reactions. Type O blood is considered the universal donor as it lacks both A and B antigens, making it compatible with all blood types. Type AB blood is the universal recipient as it has both A and B antigens, allowing it to receive blood from any type.
Process of Blood Transfusion
Blood transfusions are typically performed in a hospital setting by a qualified medical professional. The process involves the following steps:
- Blood Typing and Cross-Matching:The recipient’s blood is tested to determine their blood type and Rh factor. The donor’s blood is then cross-matched with the recipient’s blood to ensure compatibility.
- Transfusion:The donor blood is transfused into the recipient’s vein through an intravenous (IV) line. The rate of transfusion is carefully controlled to avoid complications.
- Monitoring:The recipient is closely monitored during and after the transfusion for any adverse reactions or complications.
Indications and Risks of Blood Transfusions
Blood transfusions are indicated in various medical situations, including:
- Severe blood loss due to trauma, surgery, or other medical conditions
- Anemia (low red blood cell count)
- Blood disorders, such as sickle cell anemia or leukemia
Blood transfusions are generally safe, but they carry some potential risks, such as:
- Transfusion Reactions:These can range from mild (e.g., fever, chills) to severe (e.g., anaphylaxis).
- Transfusion-Transmitted Infections:Although rare, it is possible to transmit infections, such as HIV or hepatitis, through blood transfusions.
- Iron Overload:Repeated blood transfusions can lead to iron accumulation in the body, which can cause health problems.
To minimize risks, blood transfusions are carefully monitored and used only when medically necessary.
Essential Questionnaire
What are the major components of blood?
Red blood cells, white blood cells, platelets, and plasma.
What is the function of hemoglobin?
To transport oxygen throughout the body.
How are platelets involved in blood clotting?
They aggregate and form a plug at the site of injury, initiating the clotting process.
What is the role of plasma proteins?
To maintain blood volume, transport substances, and contribute to immune function.
Why are blood transfusions necessary?
To replenish blood volume, replace lost blood cells, or provide specific blood components in cases of deficiency or disease.